

While employers are evaluating background screening services or making policy decisions about...

The patient census doesn't decrease just because you're short-staffed.
When a cardiac unit is running at 87% capacity on Thursday and you have a qualified candidate who can start Monday, every day of delay feels like an additional patient safety risk. Background checks, license verifications, and sanction screenings all take time. And when orientation is already scheduled, the pressure to accept a candidate's documentation at face value becomes almost irresistible.
"I think corners start to get cut for the sake of speed," says Matt Jaye, senior vice president of sales at Cisive, who has seen this dynamic play out at healthcare organizations over the past 25 years. "And as a result, you start to see things like this."
Impostor nurses. Fraudulent credentials. Nurses who allegedly used 20 aliases to work at nine Pennsylvania facilities. Providers accused of treating nearly 5,000 patients in Florida using a stolen license. The 7,600 fake nursing diplomas that federal investigators traced to three Florida schools in Operation Nightingale.
The impostor nurse problem isn't new. But the conditions that allow it to thrive—including staffing desperation and fragmented screening technology—have converged into what experts now recognize as a systems failure, not just individual bad actors.
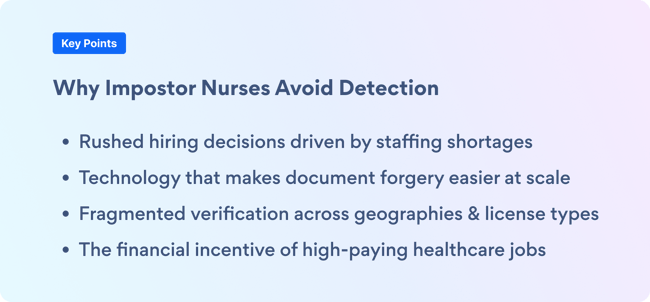
As a veteran of the background screening industry, Matt knows that healthcare fraud isn’t new. What's changed are the scale and the conditions. Three forces have converged:
"It's not just this unified agreement or license across all 50 states," Joe explains. "Understanding where someone's primary license is, where their reciprocity is, what is accepted by the accrediting bodies, and understanding those requirements is really the most fundamental part."
Here is a common scenario: A nurse is sanctioned in Texas for a serious violation. That nurse moves to Pennsylvania and applies for work using a reciprocal license. If the hiring organization only verifies the Pennsylvania license status, they'll miss the Texas sanction entirely.
"These folks are becoming smarter," Joe says. "They understand where the loopholes exist."
Beyond licensure lies additional verification challenges, including falsified immunization records, forged employment histories, and manipulated transcripts. "There's a whole ecosystem of fraud going on out there. It's not just limited to licensing,” Matt says.
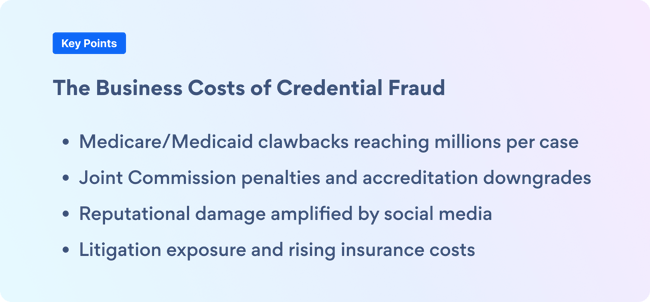
When healthcare leaders think about impostor nurses, patient safety rightfully comes first. But employers also face significant business implications.
When an impostor nurse is discovered, federal programs and financial institutions can halt future payments, but they can also demand refunds for services provided, sometimes going back years.
"Every payment issued since that time, we're now flying back," Matt explains. "You can imagine what that looks like, given the cost of healthcare. It's really, really significant."
For example, an impostor nurse works full time for two years treating Medicare and Medicaid patients, and the organization billed $500,000 for their services. All of that revenue could be clawed back.
Organizations like the Joint Commission and National Committee for Quality Assurance (NCQA) regularly audit credentialing practices.
"If they see that something's out of line, that can cost you from being a four-star facility," Matt says.
Losing accreditation status can trigger remediation plans—including more frequent audits, operational constraints, and, in severe cases, losing the privilege of serving certain patient populations.
Allowing imposter nurses to work in your organization creates reputational damage that evokes public displeasure, especially when amplified online.
Jennifer Mensik Kennedy, president of the American Nurses Association, captured the emotional impact: "You hear about those cases on social media and your heart sinks. … it shakes the trust of people."
In healthcare, trust is currency. Losing that trust affects everything from patient choice to physician recruitment to insurance contracting.
Most individuals posing as licensed nurses should be detected during initial screening, at least when organizations conduct comprehensive verification procedures. But that's where stressed-out HR teams and organizations can be vulnerable.
"In the haste and the pressure that these HR leaders and their teams are faced with, sometimes there's an inclination to say, 'Well, you know, this is taking two days, and let me just get the copy from the candidate, and we'll accept that at face value,'" Matt says.
Watch for these warning signs:
Even organizations that conduct thorough initial screening often neglect continuous monitoring. A nursing license verified on day one might expire six months later, while a clean initial background check doesn't account for criminal charges filed after hire.
"If you don't have any sort of continuous monitoring process in place, you may be taking that employee's word for it," Matt explains. "That's not good enough. That's where fraud can come in. It's easy to manipulate documents. That's where you really need actual primary source verification."
There’s a faulty assumption too many healthcare leaders make: Thoroughness takes time, and so we have to accept some risk to hire quickly.
"I think historically, that had been the case," Matt acknowledges. "But we're in an environment now where you don't have to choose between good or fast."
The difference is infrastructure. Organizations that treat background screening and credentialing as isolated, vendor-managed processes will always face the speed/thoroughness dilemma. But organizations that build verification into their core hiring systems can achieve both.
"It really is thinking differently and working with a partner that understands the full life cycle in healthcare," Joe explains. "There are very complex and compliance-driven processes, but there are also opportunities to drive significant interoperability."
The key is integration. When your background screening partner's data lives in your applicant tracking system, your HR information system, and your scheduling software, verification doesn't slow down hiring. It becomes part of the workflow.
PreCheck's integrated platform illustrates this solution. Organizations, on average, see a 31.8% reduction in time to fill while maintaining 99.9994% background check accuracy. That's solving the right problem correctly.
"We have to get our data to live in their system of record," Joe says. "The challenge is not sacrificing the efficacy of the solutions along the way."
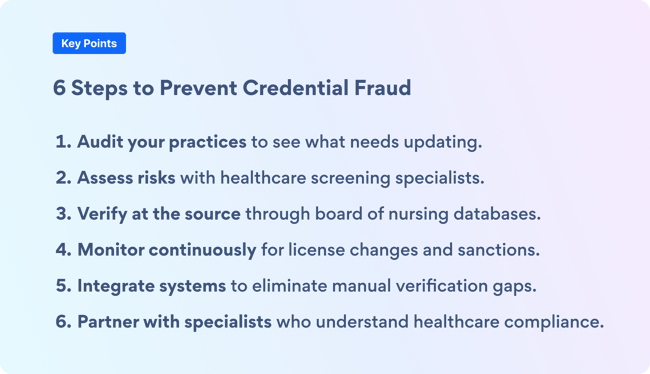
What are the next steps for organizations worried about their vulnerability? Here are six steps to take with every potential hire.
Solving the impostor nurse problem isn't about hiring teams working harder or being more suspicious. It's about building the right infrastructure before a crisis forces your hand.
"These are HR and talent acquisition leaders burdened with serious compliance challenges," Joe says. "There's help. The solutions available today weren't available five years ago. We can drive serious automation and efficiency while closing compliance gaps."
Healthcare organizations face legitimate staffing pressure. Patients still need care. But verification isn't a luxury to skip because you're busy. It's essential infrastructure, like fire suppression or infection control.
"Really trusting the pros and relying on the partners that you have that are experts at identifying these things," Matt concludes. "That's the best place to start."
With the right partner, you don't have to choose between speed and safety. You protect patients, protect your organization, and still fill critical roles quickly.
In healthcare, you can't afford to choose. You need both.
Ready to assess your organization's vulnerability to fraud? PreCheck healthcare screening experts can review your current verification processes, identify gaps, and recommend solutions that maintain compliance without slowing hiring. Talk to a compliance expert today.
Author: Jenni Gallaway
Bio: Content Marketing Manager at Cisive. 8 years of experience in the background screening industry.
Let's Connect on LinkedIn
While employers are evaluating background screening services or making policy decisions about...

Healthcare organizations face a dual challenge: filling critical positions quickly while ensuring...

Did you know that only 17% of employers screen their employees at least annually? However, with the...